A recent announcement about a vaginal ring to prevent HIV has Aids activists and women’s sexual and reproductive health advocates excited. But where would this ring fit in South Africa’s HIV prevention programme? Amy Green investigates.
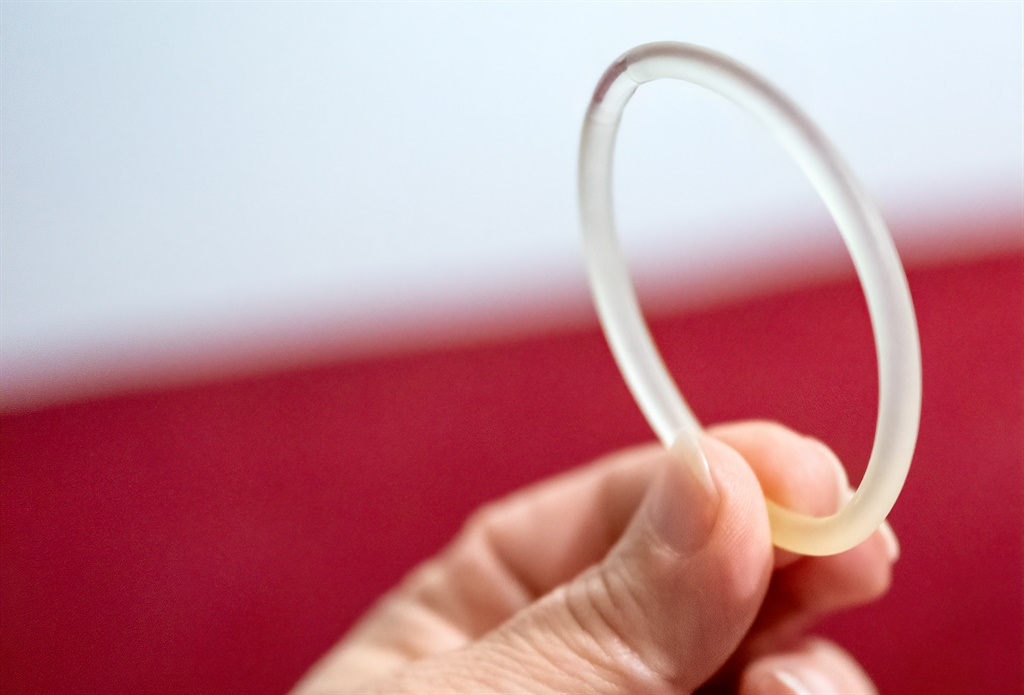
Just days before the start of Women’s Month, the European Medicines Agency (EMA) delivered a positive opinion on a vaginal ring to prevent HIV. The ring, intended to be inserted once-monthly, contains the antiretroviral dapivirine and was developed by the non-profit organisation the International Partnership for Microbicides (IPM).
IMP’s Dr Zeda Rosenberg described the product as the very first long-acting HIV prevention tool “designed to help women manage their HIV risk on their own terms”.
This paves the way for the ring to be prequalified by the World Health Organisation (WHO) and the anticipated adoption of the ring by countries after national regulatory approvals.
Read: Women in Africa could soon access dapivirine ring, which reduces risk of HIV
IPM, and others in the field, have lauded the EMA announcement as a “milestone for women’s HIV prevention”.
First in prevention specifically designed for women
Despite the significantly higher risk for HIV infection faced by women, particularly in sub-Saharan Africa, the world has not seen an HIV prevention option specifically designed for women since the female condom was approved nearly three decades ago.
Earlier hopes for a vaginal gel (microbicide) containing the ARV tenofovir were dashed when the gel failed to prevent sufficient HIV infections in pivotal studies.
At around 25%, HIV prevalence in women aged 15 to 49 in South Africa is roughly double that of men in the same age group, according to estimates from the Thembisa mathematical model on the epidemic.
Currently, South Africa’s HIV prevention strategy hinges mainly on three tools – condoms, oral PrEP (pre-exposure prophylaxis) and expanding access to ARV treatment (ART). But activists and experts said there were issues with all three methods – especially for women due to a combination of biological and societal factors.
For example, some research has shown women in a largely patriarchal society often struggle to negotiate condom use with male partners who hold the power.
Women face a similar dilemma when it comes to oral PrEP, which comes in the form of a daily pill. It contains the ARV truvada, which HIV negative individuals who are at high risk of HIV infection can take as a means of prevention. PrEP is effective at preventing HIV – close to 100% – if taken as prescribed.
However, it is not very discrete and women have reported that they struggle to hide the pills from partners who do not know they are taking them.
Hits and misses with PrEP
Moreover, access to PrEP in South Africa is “dismal” at best, according to long-standing HIV activist and director of advocacy for prevention of HIV and Aids, Yvette Raphael.
This is despite the health department’s ambitious plans to roll-out PrEP across the country as announced in February this year.
These targets included making PrEP available in every community health centre and clinic by the end of next month. By the end of March, the department’s target was to have the HIV prevention pill available in at least one health facility in each sub-district.
Admittedly, the department set its targets before the Covid-19 coronavirus pandemic hit South Africa.
However, the department has been criticised for its Covid-19 response – particularly with the continued running of critical and life-saving health programmes and services, especially those related to HIV and TB.
Read more: TB and HIV patients are not collecting their meds
This limited access to care sparked warnings from clinicians, including professor Francois Venter, that: “Far more people are going to die because of the inadequate response to Covid-19 than the virus itself.
“Covid-19 has interrupted everything. We shouldn’t have allowed this. Our gains when it comes to HIV and TB will sadly be reversed because of the Covid-19 disaster and how government has responded,” said Venter, the deputy executive director of the Wits University Reproductive Health and HIV Institute.
The health department confirmed that the PrEP roll-out has not happened as planned.
“The scale-up of PrEP in public health facilities did not proceed at the pace it was scheduled due to the disruptions resulting from the Covid-19 pandemic and the lockdown regulations,” Popo Maja, spokesperson for the health department, told Spotlight.
“Currently there are more facilities offering PrEP. Although the aim was to scale-up PrEP in at least one facility per district, there are some districts in the Northern Cape, Limpopo and the Western Cape where this is not the case. [In the other six provinces] most, if not all districts, have at least one public clinic offering PrEP.”
However, Maja said that the number of people taking PrEP has increased over this period. In February, the department reported that 50 000 people had been started on PrEP over the last four years. Maja told Spotlight that this figure has increased to 70 000.
“Covid-19 did affect PrEP during April and May when we experienced a dip in the uptake of PrEP. By June we saw the demand for PrEP increase to 128% of the average month’s uptake. Various strategies were also put in place to ensure that those on PrEP could remain on PrEP through decentralised pick-up points, multi-month prescriptions, social media, web-based and online support tools,” he said.
Gender, HIV and choice
When it comes to treatment as a prevention strategy, heterosexual women are also disadvantaged as data shows HIV-positive men are significantly less likely to be on ART than HIV-positive women.
According to Venter, women make up just under 70% of South Africa’s ART programme – one of the highest gender disparities in the world.
“We almost have two different countries in terms of gender and HIV success in South Africa. The UNAids 90-90-90 targets were probably achieved a few years ago for women. Men are woefully left behind and nowhere near any of the targets,” explained Venter.
The UNAids targets are that, by this year, 90% of people living with HIV know their status, 90% of people diagnosed with HIV are taking ART and that 90% of people on ART have achieved viral suppression (meaning there is not enough virus in the blood to transmit HIV to others).
Moreover, during the Covid-19 pandemic there have been multiple reports of people unable to access ARVs.
“Since the lockdown, what’s happened is people who have gone to facilities are likely not receiving the services they need, which have impacted heavily on access to ARVs,” said Tshepo Maboe, acting manager for the Treatment Action Campaign in Gauteng.
Dr Thesla Palanee, who heads network trials at Wits Reproductive Health and HIV Institute, said compared to existing methods, the dapivirine ring offers a potential solution to women as it is more discrete and can be hidden from male partners.
“We all know women like choices. Like in the contraceptive field there are a range of options to prevent pregnancy – from condoms, to the oral pill, to injectables to long-acting intra-uterine devices.
“With a range of options, women can choose one or the other over the course of their lifespan. Similarly, we need a range of options for women when it comes to protecting themselves from HIV,” Palanee said.
Said Venter: “The benefit of the ring is you don’t have to remember to swallow a tablet every day.”
Questions on efficacy
Some people have asked what the ring’s role in HIV prevention should be, considering it only showed around a 30% efficacy rate in trials.
Venter explained that there are inherent difficulties measuring actual efficacy rates in phase three randomised control trials because researchers cannot ensure study participants use the medicines or tools exactly as directed.
According to Venter, because of this, the initial studies done on oral PrEP showed an efficacy rate of about 50%. It was only in later trials among select high-risk populations that it was found that oral PrEP was more than 90% effective.
“My instinct is that the efficacy of the ring is much higher [than 30%] but not as high as oral PrEP, however it is not insignificant. With PrEP, as I anticipate will also be the case for the ring, we get better adherence in the real world versus in clinical trials,” he said.
He noted that adherence rates for oral PrEP are much higher in the highest risk groups such as sex workers, injecting drug users and gay men.
Rosenberg told Spotlight that the ring can’t possibly be as effective as oral PrEP, even if used correctly, because it only protects against transmission through vaginal sex – and not for transmission via anal sex or injecting drug use.
“We want women to choose oral PrEP, but if they can’t or won’t use it then the ring is an excellent alternative option,” she said.
The way forward
“Once WHO prequalification is available, the health department will welcome the rapid registration of the dapivirine ring by the SA Health Products Regulatory Authority (Sahpra) so that it can be offered as an additional prevention option to women at risk of HIV infections.
“The Sahpra approval is not necessarily dependent on WHO prequalification so the application can be submitted, however, the department will wait for WHO prequalification before implementation,” Rosenberg said.
Note: The Treatment Action Campaign is mentioned in this article. Spotlight is published by Section27 and the TAC, but is editorially independent, an independence that the editors guard jealously. Spotlight is a member of the SA Press Council.
This article was produced by Spotlight – health journalism in the public interest.
| ||||||||||||||||||||||||||||||
 |




 Publications
Publications
 Partners
Partners









